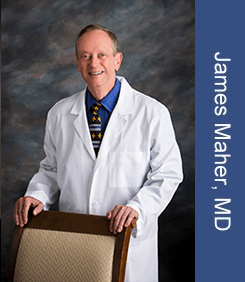
If you are looking for a reliable gasterologist in Houston, TX, you have probably come across a lot of doctors advertising their skills. A gasterologist is a type of specialist doctor who diagnoses and treats problems with the gut system. We’re proud that Katy Stomach Doctor offers a wide range of services, from consultations to expert treatments for a wide range of digestive problems. Our board-certified gasterologist, Dr. James Maher, is in charge of making sure that patients in Katy, TX, and all over Texas get the best care possible.
Who is a Gasterologist Houston, TX?

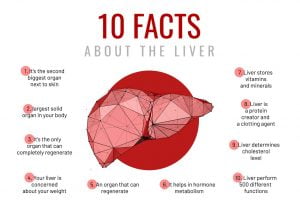
A gasterologist is a doctor who focuses on digestive system issues and how to fix them. There are bile tubes, the esophagus, the stomach, the small intestine, the large intestine (colon), and the pancreas in this part of the body. At Katy Stomach Doctor, we know how to treat a lot of different conditions, from mild ones like hemorrhoids to more important ones like colon cancer and hepatitis. Endoscopic treatments, in which special tools are used to look inside the digestive system, can only be done by gastroenterologists.
Scope and Significance of a Gasterologist’s Work
A gasterologist does a lot more than just figure out what’s wrong with gut systems. They are very important for finding, preventing, and treating many illnesses that can have a big effect on your health and quality of life. As part of their job, they do, but are not limited to,
- Early discovery and prevention: To avoid diseases like colon cancer, it’s important to get regular screenings and use early detection methods. Gasterologists do colonoscopies to find polyps and remove them before they turn into cancer.
- Diagnosis and Treatment: To find out what’s wrong with people, like those with hepatitis, Crohn’s disease, or ulcers, they use a variety of diagnostic tools, such as blood tests, imaging studies, and endoscopic methods. Treatments can include managing medications and giving advice on how to live a healthier life.
- Managing Long-Term Conditions: Irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) are two GI conditions that need ongoing care. Gasterologists make long-term care plans for each patient that are specific to their needs.
- Medical interventions: Most treatments do not involve surgery, but in some cases, surgery may be needed. Gasterologists work with doctors to make sure that patients get the best care possible.
- Teaching patients: One of the most important parts of a gasterologist’s job is teaching patients. They teach patients how to take care of their conditions by making changes to their food, lifestyle, and medications in order to reduce symptoms and improve quality of life.

Conditions Treated by Gasterologist at Katy Stomach Doctor
At Katy Stomach Doctor, under the adept leadership of Dr. James Maher, we provide a multitude of services addressing various gastrointestinal conditions, including but not limited to:
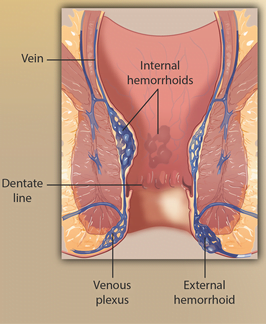
1. Hemorrhoids: We let people with painful and annoying hemorrhoids choose between non-surgical and surgical treatments.
2. Colon Cancer: Screening colonoscopies are used to find and treat colon cancer as soon as possible.
3. Hepatitis: Different kinds of hepatitis can be managed and treated in ways that aim to fix liver damage and make the liver work better.
4. Bacterial Infections: To treat bacterial infections effectively, they need to be correctly diagnosed and treated with antibiotics.
5. Other Conditions: We also treat Crohn’s disease, ulcerative colitis, gastric reflux disease (GERD), and peptic ulcers, among other stomach issues.
Why Choose Katy Stomach Doctor?
Katy Stomach Doctor is the best place to find a doctor in Houston, TX If you need one. They hire people with a lot of knowledge and work with a well-known health system. Board-certified in gasterology, Dr. James Maher is the most skilled and kind person who runs our office.
1. Comprehensive Services: We provide all gastroenterology services, from the first appointment to treatment and review.
2. Expertise and Experience: Dr. Maher’s extensive experience allows us to diagnose and treat various gastrointestinal conditions accurately.
3. Convenient Location and Hours: Our clinic, located in Katy, TX, is accessible to patients across Texas. It is open Monday through Thursday from 8:30 AM to 5:00 PM and Friday from 8:30 AM to 2:00 PM.
4. Affiliation with Memorial Hermann Hospital System: As part of this world-renowned network, our patients benefit from the latest medical innovations and comprehensive care options.
FAQs About Gasterologist Houston, TX
1. How often should I get a colonoscopy?
It is important to get regular tests to find colon cancer early. Screenings for most people should start at age 45 and happen every ten years after that. But if you have a history of colon cancer in your family or other risk factors, Dr. James Maher may suggest that you get screened more often.
2. What symptoms should prompt a visit to a gasterologist?
You should see a gasterologist if you have serious heartburn, jaundice, diarrhea, abdominal pain that won’t go away, or weight loss that you can’t explain. If you have any of these signs, you should see a doctor right away to rule out and treat possible digestive problems.

Your Digestive Health Matters: Partner with Gasterologist Houston, TX
The gut is a very complicated structure that is needed for good health. Your quality of life can be greatly affected when it’s not working right. That’s why Katy Stomach Doctor is there.
Doctor James Maher leads our team of experienced gasterologists who are committed to providing complete and individualized care for a wide range of stomach problems. Whatever you need, from basic check-ups to complicated treatments, we have the skills and tools to do it.
We know that dealing with stomach problems can be overwhelming. We work hard to make sure our patients are in a safe and comfortable place because of this. The state-of-the-art facilities and caring staff at our company promise that you will get the best care possible.
Take back control of your life from stomach problems. To get healthy, make an appointment with Katy’s Stomach Doctor. Let us help you have the healthiest gut and body possible.
Please contact us or visit our office to learn more about our services or to schedule an appointment.
We work with several insurance plans and can make appointments that work with your busy schedule.
Your digestive health deserves the best care. Choose Katy Stomach Doctor.
Houston, TX fun facts:
• It was the world’s first multi-use dome-shaped sports stadium. It is now broken.
• Matt Stone, who made South Park, was born in Houston.
• It has more than 62,000 works of art, making it the biggest museum in Texas and the most extensive collection in the Southwest U.S.